- September 6, 2023
- LASIK
Your Vision, Our Passion
Laser
Accurate
Xenial
Modern
Innovative

Laxmi Eye Hospital & Institute
With leading Eye hospital in Panvel, Kharghar, Kamothe & Dombivli. We are one of the largest chains of eye hospitals in Mumbai. Known for our excellence in the eye care industry for more than 30 years.
Experienced eye doctors & transparency in treatment is what we are known for. We offer best-in-class diagnostic and sophisticated eye care treatment in Panvel, Kharghar, Kamothe & Dombivli. Let it be Cataract, Lasik, Glaucoma or Retina Treatment, Laxmi Eye Institute offers comprehensive eye care under one roof at affordable cost.
We have the best team of eye specialists from all across India to cater simple or complex eye problems.
30+ Years of Experience
We have been providing services to patients for over 30 years.
Experienced Doctors
We have a team of highly skilled and experienced doctors.
Advanced Healthcare
We utilize advanced healthcare technologies to provide state-of-the-art eye care services.
20L+ Satisfied Patients
We have a heritage of quality eye care spanning 3 decades and over 20 lakh happy patients.

Know More About Us
Laxmi Eye Clinic is a specialized healthcare facility that offers comprehensive eye care services. The clinic provides a wide range of treatments, including cataract surgery, glaucoma treatment, and refractive surgery. The clinic is equipped with state-of-the-art technology and staffed by experienced ophthalmologists who are dedicated to providing the best possible care to their patients. Laxmi Eye Clinic also offers regular eye check-ups and preventive care services to help maintain healthy vision. The clinic is known for its patient-centered approach and commitment to excellence in eye care.
- Cutting-edge eye Hospital offering advanced diagnostic and treatment technology
- Team of highly skilled ophthalmologists, optometrists, and support staff
- Comprehensive range of services including routine exams, complex surgeries, and laser vision correction
- Commitment to putting patients first and ensuring their comfort and satisfaction
- Focus on achieving and maintaining optimal eye health for a better quality of life
Training At Laxmi
Laxmi Eye Institute has one of the longest-running and most reputed cataract surgical training programs that includes SICS and Phacoemulsification. Our program has a well-organized schedule for academics and practical training. Academic training includes a rigorous schedule of presentations, seminars, case discussions, and journal club presentations. The course follows all the norms of admission and conduct as laid down by the National Board of Examinations, New Delhi.
Hands-on Surgical Training At Laxmi Eye Institute-

Why Choose Us
Laxmi is the preferred eye care service provider in the regions where we operate ( Panvel, Kharghar, Kamothe & Dombivli ). Our patients testify to the unmatched ethical standards and care by our team of eye specialists and support staff at every centre of Laxmi Eye Institute.
-
1
Complete Family Care
Never compromise on your eye health. Visit the top Eye hospital in Mumbai, Laxmi Eye Institute, (Panvel – Kharghar - Kamothe – Dombivli) -
2
Training Program
Laxmi Eye Institute has one of the longest-running and most reputed cataract surgical training programs that includes SICS and Phacoemulsification. -
3
International Patients
Laxmi has the best-designed operation theatres coupled with surgical suites aimed at maximizing patient comfort and safety. That makes it the best Eye Hospital in Navi Mumbai & Mumbai.


Choose The Best For Your Eyes!
Cataract Surgery
We at Laxmi offer different types of cataract surgeries and different types of lens. Patients can avail Cataract treatment in Navi Mumbai, Panvel, Kharghar, Kamothe & Dombivli at Laxmi Eye Institute at affordable cost.
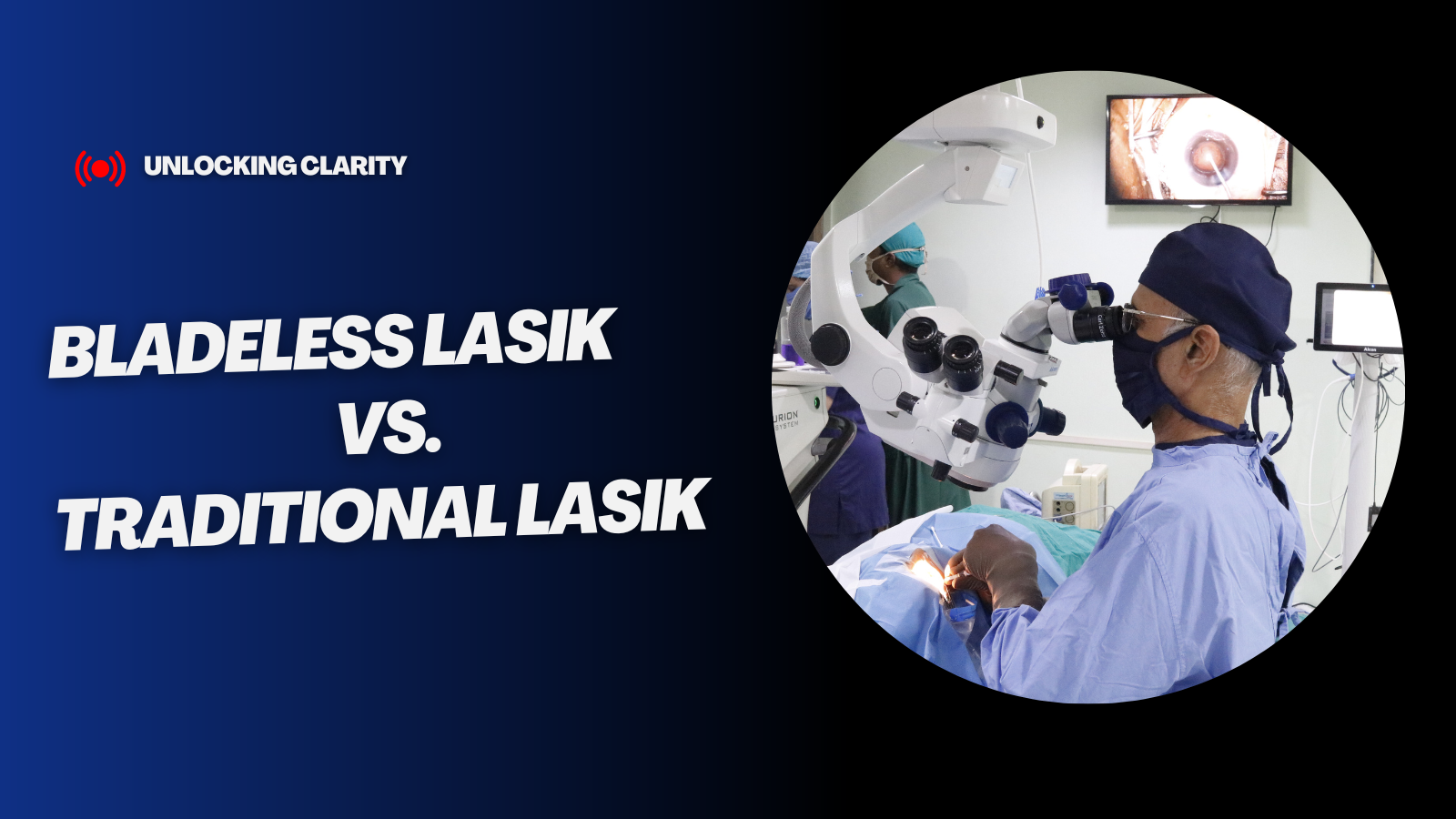
Read MoreLasik Surgery
Are you looking for a Lasik or Bladeless Lasik or Contoura Lasik treatment? It’s important to mention here, opt for Lasik only if you are the right candidate for it! We at Laxmi offer advanced Lasik treatment at an affordable cost.
Read MoreCornea Clinic
A qualified and experienced cornea specialist coupled with latest technology being used in ophthalmology can accurately map and quantify each and every layer of the eye giving the Ophthalmologist proper insight into the disease.
Read MoreThe most frequent reasons that patients visit Laxmi Eye Hospital
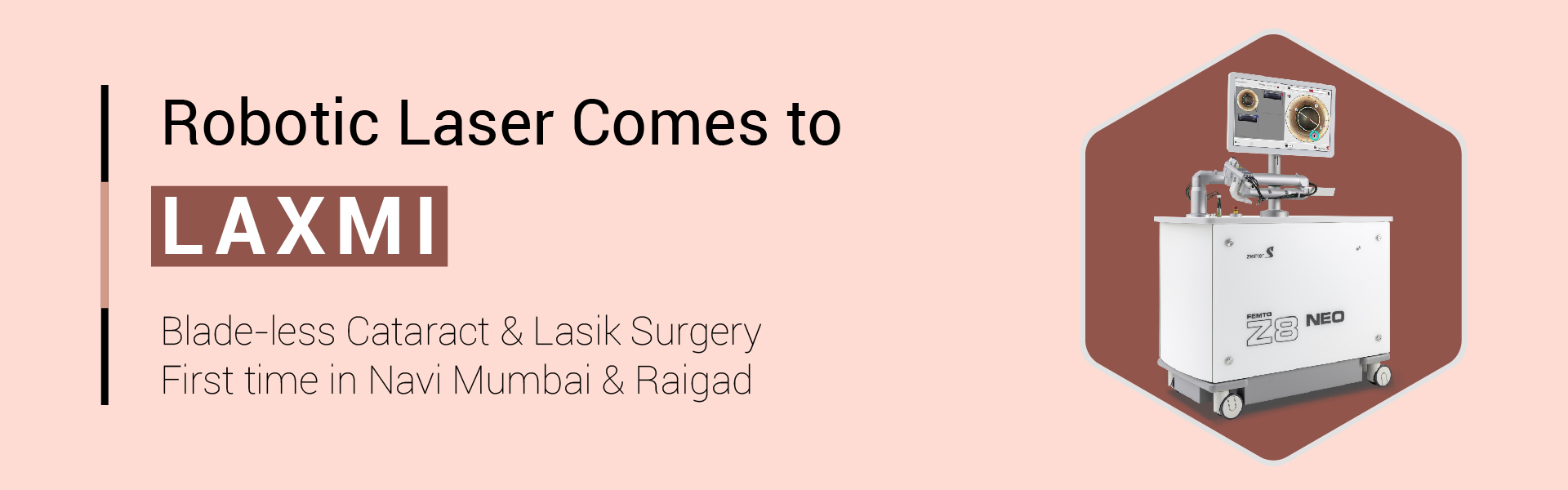
Robotic Laser at Laxmi
With the use of advanced software and sensors, the robotic laser at Laxmi can perform complex tasks with unparalleled precision. The Femto z8 machine is one of the latest advancements in this field, offering even higher levels of accuracy and efficiency. Your safety and wellbeing are our highest priorities. This is why we chose the Ziemer FEMTO LDV Z8, a unique laser which offers the following features: It’s the first and only femto second laser that works in the nano Joule range which means that it is even gentler for the eye. The Swiss-made optics enable for even more precision than with other lasers. This means that surgery is faster, safer and more comfortable.

Make An Appointment
Some easy steps to get your proper solution
Search Doctor
Check Doctor Profile
Doctor Appointment
Get First Solution
Educational Videos
Patient Testimonials
All Copyright© Reserved @Laxmi Eye Hospital And Institute